President Biden’s January 28th executive order to reopen enrollment in the federal ACA Marketplace from February 15 through May 15, combined with $50 million in federal spending on outreach and education about ACA coverage options, has the potential to reach millions of people who were uninsured prior to or have lost coverage during the pandemic. As of 2019, there were 29 million non-elderly uninsured people, and the majority (57%) were eligible for financial assistance through the ACA Marketplaces (33%) or Medicaid (25%). KFF estimates indicate that nearly nine million uninsured people could be eligible for free or subsidized Marketplace coverage during the new enrollment period. Importantly, these actions to facilitate enrollment in ACA Marketplace coverage will also likely lead eligible low-income people to enroll in Medicaid coverage.
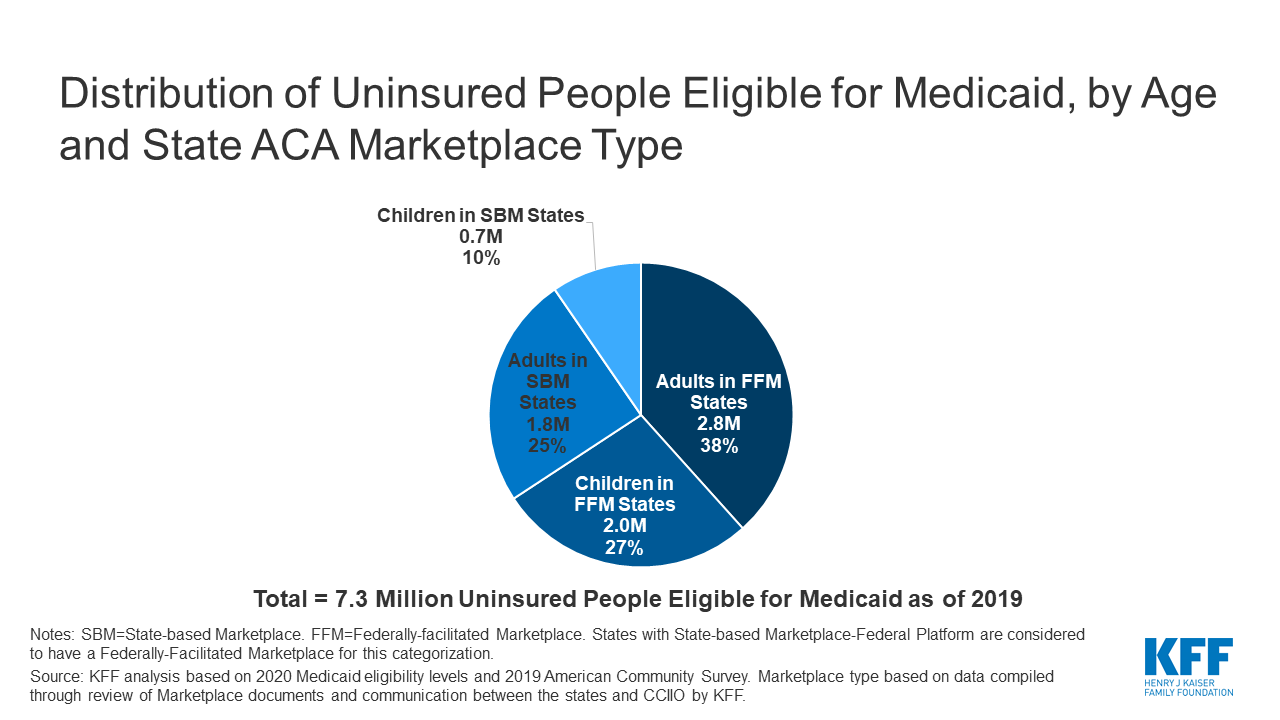
Prior to the pandemic, 7.3 million uninsured people were eligible for Medicaid. Nearly two-thirds of these people are children (27%, or 2.0 million) or adults (38%, or 2.8 million) living in the 36 states in which the ACA Marketplace is federally-operated (FFM) or state-operated but the state uses the federal Healthcare.gov platform (SBM-FP) and will reopen for enrollment under the executive order (Figure 1). During 2020, all but one of the State-based Marketplace (SBM) states reopened Marketplace enrollment due to the pandemic. In response to the reopening of the federal Marketplace, 11 of the 15 SBM states have announced similar enrollment periods.
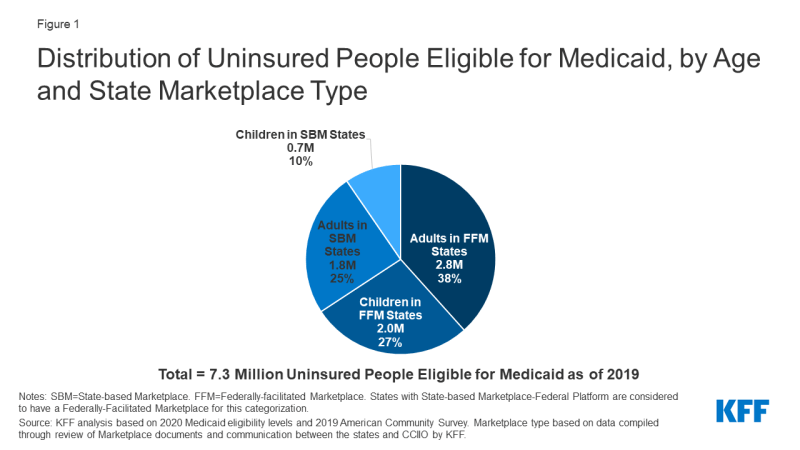
Figure 1: Distribution of Uninsured People Eligible for Medicaid, by Age and State Marketplace Type
Under enrollment simplification processes established by the ACA, states must provide a single application for Medicaid, CHIP, and Marketplace coverage, thereby establishing a “no wrong door” application process for ACA coverage. This process means that the Marketplaces will screen or assess individuals’ eligibility for all health coverage programs, including Medicaid and CHIP, and individuals will be enrolled in or referred to the program for which they are eligible regardless of how they apply. Most states utilizing the FFM do not authorize the FFM to make final Medicaid eligibility determinations for most groups, but instead conduct full eligibility determinations for individuals after the FFM assesses them as eligible for Medicaid. The states that operate SBMs typically have a single integrated system through which individuals can apply for and renew Medicaid, CHIP and Marketplace coverage.
In recent Marketplace open enrollment periods, nearly a million people who applied for ACA coverage through the FFM have been assessed eligible for Medicaid, and millions more who apply through SBMs are determined eligible. During the 2020 Marketplace open enrollment period (which closed in December 2019), 836,451 people who applied for ACA coverage through the FFM, or 8% of all applicants, were assessed or determined eligible for Medicaid. The number was down slightly from the 952,049 during the 2019 open enrollment period and much lower than the 1.2 million assessed/determined eligible during the 2016 open enrollment period. Large reductions in funding for marketing, outreach, and in-person enrollment assistance have likely contributed to declines in Marketplace applications and enrollment since 2016. During the 2016 open enrollment period, the last year for which complete data on SBMs was reported, more than 4 million people who applied for coverage through the Marketplace were determined eligible for Medicaid, though that number includes some people who intended to apply for Medicaid and has likely declined in recent years as Marketplace applications and enrollment have stabilized.
Investments in outreach and advertising as well as enhanced funding for in-person assistance to support the new Marketplace enrollment period can also raise awareness of Medicaid and promote Medicaid enrollment. Findings from a consumer survey reveal most people are unaware of ACA-related coverage options, including whether their state has expanded Medicaid, and lack basic information on how to apply. And, many who do apply for Marketplace or Medicaid coverage face challenges with the application process. Expansive advertising campaigns coupled with targeted outreach strategies during the new enrollment period can educate consumers on the availability of both Marketplace and Medicaid coverage. In addition, supplemental funding for federal navigators would enable them to respond more quickly to provide in-person help to both Marketplace and Medicaid enrollees.
While much attention has been paid to the importance of expanding eligibility to the over 2 million people in the Medicaid coverage gap, who currently have no affordable coverage option, it may be possible to make gains in Medicaid coverage by reaching those who are eligible but not enrolled. Ongoing efforts to expand ACA Marketplace coverage may reach some of these individuals.