Introduction
Across states, health and long-term care workers and residents have been the first groups offered COVID-19 vaccines, consistent with federal recommendations. Previous KFF analysis estimated that, nationwide, 19.7 million adults work in health and long-term care settings, of which roughly 15.5 million are estimated to have direct patient contact and be included in the initial priority group for vaccination. Media reports suggest that the initial vaccination efforts have been slower than expected and that some health care workers who have been offered the vaccine have chosen not to get vaccinated, particularly among staff in long-term care facilities. More information is needed to understand why some health care workers are declining the vaccine, although there are anecdotal reports of concerns about safety and/or side effects. KFF survey data show that roughly three in ten health care workers (29%) express hesitancy about getting the COVID-19 vaccine and that, among all adults, levels of vaccine hesitancy and reasons for hesitancy vary across demographic groups.
This analysis provides an overview of demographic characteristics and health insurance coverage of health care workers with direct patient contact, including those working in hospital and long-term care settings, who may be most at risk of patient contact with someone with coronavirus due to the concentration of cases in these facilities. Increased understanding of who these health care workers are can help inform vaccination efforts and prevent disparities in vaccination among this group.
Findings
Table 1 presents data on race/ethnicity, citizenship status, sex, age, education, poverty status and health insurance coverage for the 15.5 million health and long-term care workers who are estimated to have direct patient contact. It also includes separate data for those working in hospitals and long-term care facilities, who account for 37% and 25% of health care workers with direct patient contact, respectively.
Overall, the data show that, although most of these health care workers are White (59%) and citizens (95%), 41% are people of color and 5% are noncitizens. The majority are women (77%), and nearly one in four (23%) are age 55 or older. Most have completed at least some college (80%), and, reflecting that they are all employed, few are low-income (17%) and nearly all have health insurance coverage (93%). Hospital workers largely mirror these overall patterns, although they have higher levels of education, income, and health coverage. Workers in long-term care settings include higher shares of people of color (52%), non-citizens (8%), women (84%), and workers age 55 or above (27%) and have lower levels of educational attainment, lower incomes, and higher uninsured rates compared to the overall population of health care workers with direct patient contact. More detailed findings include:
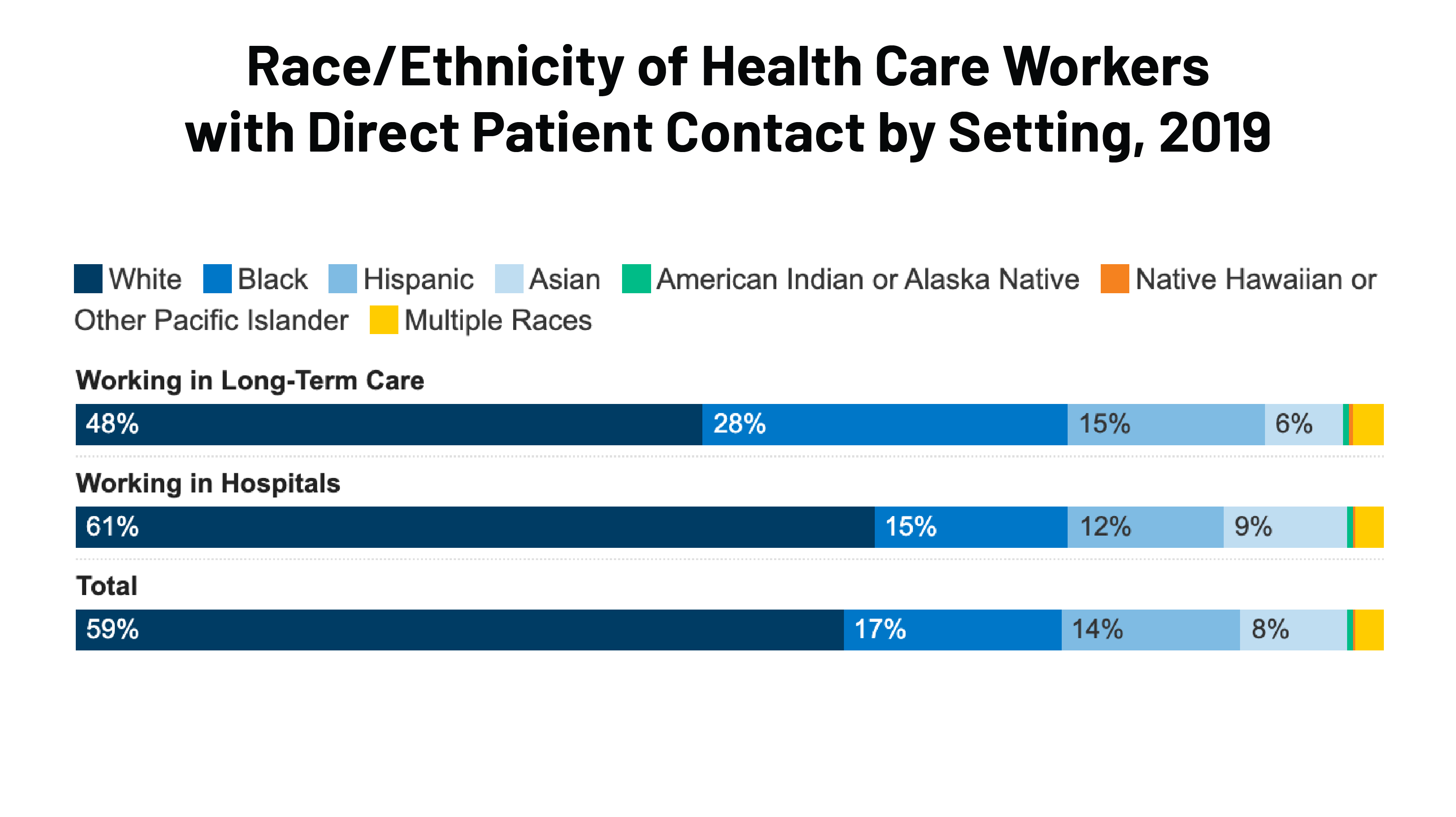
Race/ethnicity. Roughly six in ten health care workers with direct patient contact are White (59%), while the remaining 41% are people of color, including 17% who are Black, 14% who are Hispanic, and 8% who are Asian (Figure 1). Among those working in long-term care settings, over half (52%) are people of color, including over one in four (28%) who are Black.
–
Citizenship Status. The large majority of health care workers with direct patient contact are citizens (95%), while 5% are noncitizens (Figure 1). However, the share who are noncitizens is higher, at 8%, among those working in long-term care settings.
Sex. Over three-quarters (77%) of health care workers with direct patient contact are women, and this share rises to 84% among those working in long-term care settings.
Age. Nearly a quarter (23%) of health care workers with direct patient contact are age 55 or older, while four in ten (41%) are age 35-54 and over one-third (35%) are below age 35. Those working in long-term care settings include a slightly higher share of workers age 55 or above (27%), while those working in hospital settings have a slightly lower share of workers age 55 and older (21%).
Education. Eight in ten of health care workers with direct patient contact have completed at least some college, including 45% who have a bachelor’s degree of higher (Figure 1). Education levels are higher among hospital workers, with nearly nine in ten (88%) completing at least some college, including over half (54%) who have a bachelor’s degree or higher. In contrast, among those working in long-term care, six in ten have completed some college, with only 20% having a bachelor’s degree or higher and 10% having less than a high school education.
Poverty Status. Overall, 17% of health care workers with direct patient contact are low-income (household income less than 200% of the federal poverty level (FPL)), with only 5% with household income below the poverty level (Figure 1). Over half (54%) have income at 400% FPL or higher. Those working in hospitals generally have higher incomes, with nearly two-thirds (64%) having household income at 400% FPL or higher. Household income is lower among those working in long-term care, where one-third (33%) are low-income, including 11% who have household income below poverty.
Health Insurance Coverage. Less than one in ten (7%) health care workers with direct patient contact are uninsured (Figure 1). Nearly eight in ten (79%) have private health insurance coverage, 10% are covered by Medicaid, and 4% have Medicare coverage. Coverage rates are higher among those working in hospitals, with only 3% uninsured and 90% having private coverage. In contrast, coverage rates among those working in long-term care are lower, with 14% uninsured. Moreover, they have higher rates of Medicaid coverage (21%) and lower rates of private insurance (60%).
| Total | Working in Hospitals | Working in Long-Term Care | |
| Total (millions) | 15.5 | 5.8 | 3.8 |
| Race/Ethnicity | |||
| White | 58.6% | 61.0% | 48.0% |
| Black | 16.6% | 14.9% | 27.9% |
| Hispanic | 13.8% | 11.9% | 15.1% |
| Asian | 8.0% | 9.4% | 5.9% |
| American Indian or Alaska Native | 0.5% | 0.4% | 0.6% |
| Native Hawaiian or Other Pacific Islander | 0.2% | 0.2% | 0.2% |
| Multiple Races | 2.2% | 2.2% | 2.4% |
| Citizenship Status | |||
| Citizen | 94.8% | 95.7% | 91.7% |
| Noncitizen | 5.2% | 4.3% | 8.3% |
| Sex | |||
| Male | 22.6% | 23.6% | 15.7% |
| Female | 77.4% | 76.4% | 84.3% |
| Age | |||
| 19-25 | 11.1% | 9.8% | 12.5% |
| 26-34 | 23.9% | 26.3% | 18.8% |
| 35-54 | 41.8% | 42.5% | 40.8% |
| 55-64 | 16.9% | 17.1% | 19.2% |
| 65+ | 5.9% | 4.1% | 7.7% |
| Education | |||
| Less than high school | 3.9% | 2.1% | 9.8% |
| High school graduate | 16.0% | 9.8% | 29.7% |
| Some college | 35.6% | 33.7% | 40.0% |
| Bachelor’s or higher | 44.6% | 54.4% | 20.5% |
| Federal Poverty Level (FPL) | |||
| <100% FPL | 5.4% | 2.8% | 11.5% |
| 100-199% FPL | 12.0% | 7.5% | 21.5% |
| 200%-399% FPL | 28.7% | 25.6% | 34.9% |
| 400%+ FPL | 54.0% | 64.0% | 32.2% |
| Health Coverage | |||
| Uninsured | 7.2% | 3.1% | 13.6% |
| Private | 78.5% | 89.6% | 59.6% |
| Medicaid/Other Public | 10.2% | 5.2% | 20.9% |
| Medicare | 4.0% | 2.0% | 5.8% |
| Notes: Totals may not sum to 100% due to rounding. Persons of Hispanic origin may be of any race but are categorized as Hispanic; other groups are non-Hispanic. Medicaid/Other Public includes those covered by Medicaid, Medical Assistance, Children’s Health Insurance Plan (CHIP) or any kind of government-assistance plan for those with low incomes or a disability; people who have both Medicaid and another type of coverage, such as dual eligibles who are also covered by Medicare; and people covered under the military or Veterans Administration. Private includes those covered through a current or former employer or union, either as policyholder or as dependent and those covered by a policy purchased directly from an insurance company, either as policyholder or as dependent Source: KFF Analysis based on 2019 American Community Survey |
|||
Discussion
Increased understanding of who health care workers with direct patient contact are can help inform vaccination efforts and prevent disparities in vaccination among this group. In sum, these findings show that the roughly 15.5 million health care workers with direct patient contact are a racially diverse workforce. They are predominantly female, with most between ages 35-54. Most have completed at least some college and, reflecting their employment, few are low-income, and the large majority have health insurance. However, those working in long-term care settings are more likely to be Black and have lower levels of education, income, and insurance coverage, which may have implications for access to the COVID-19 vaccine and willingness to get vaccinated.
KFF survey data show, as of December 2020, roughly one in three adult health care workers (29%) said they probably or definitely would not get vaccinated, similar to the share among adults overall (27%). Data also show that levels of vaccine hesitancy vary across demographic groups. For example, adults age 30-49 and Black adults have relatively high levels of hesitancy, while adults ages 65 and older report greater willingness to get the vaccine. Hesitancy varies among health care workers in similar ways. For example, an earlier KFF/The Undefeated survey found that, among adults who are health care workers or who live in a household with a healthcare worker, Black adults were much less likely to say they would definitely get vaccinated compared to White adults (24% vs. 46%). Moreover, different groups have different reasons for vaccine hesitancy. For example, among adults overall who say they probably or definitely won’t get vaccinated, Black adults are more likely than White adults to cite concerns about side effects and the newness of the vaccine, and about half of Black adults in this group cite worries they may get COVID-19 from the vaccine or that they don’t trust vaccines in general as major reasons.
People living in immigrant families and people who are uninsured may also have specific concerns which could make them less likely to seek vaccination. For example, people living in immigrant families may have concerns about potential negative effects on their or a family member’s immigration status. People who are uninsured are less likely to have an established relationship with a health care provider and generally have greater concerns about potential costs of health care.
Addressing concerns and potential access barriers to vaccination among health care workers will be particularly important since, as one of the first groups offered the vaccination and a top trusted messenger for information on the COVID-19 vaccine, their experiences and take-up may help inform the general public’s attitudes and willingness to get the vaccine. Together these data suggest that providing information to respond to concerns about potential side effects and safety of the vaccine is key, particularly among Black health care workers. Clearly communicating that personal information collected for vaccination cannot be used for immigration-related purposes may help reduce fears among noncitizen workers. Moreover, ensuring people know that they will not face any costs associated with the vaccine may reduce concerns among people who are uninsured. Beyond providing education and information, making the vaccine easily accessible is key. While many health care workers are able to access the vaccine directly through their employment site, ensuring it is available in ways that accommodate workers’ varied schedules, caregiving responsibilities, and transportation options can help reduce potential access barriers among those who need to obtain it through pharmacies or community sites.