In March 2024, the Centers for Disease Control and Prevention (CDC) updated its recommendations for how people can protect themselves and their communities from respiratory viruses, including COVID-19. Following the lead of some state governments and other countries, the updated recommendations do not instruct people with COVID-19 to isolate after testing positive, in effect treating COVID more like the flu. The new CDC guidance brings a unified approach to the risks from respiratory viruses and reflects the nation’s progress against severe illness from COVID-19. However, as the nation moves further from the COVID-19 pandemic, rates of long COVID remain steady and 7% of all adults—roughly 17 million people—reported currently having long COVID in March 2024. The latest data show that rates of long COVID have remained relatively consistent for the last year, suggesting they may persist indefinitely unless new forms of prevention or treatment are discovered.
This issue brief describes the most recent trends in how many people have long COVID, rates of activity limitations among people with long COVID, and which groups have the highest rates of long COVID.
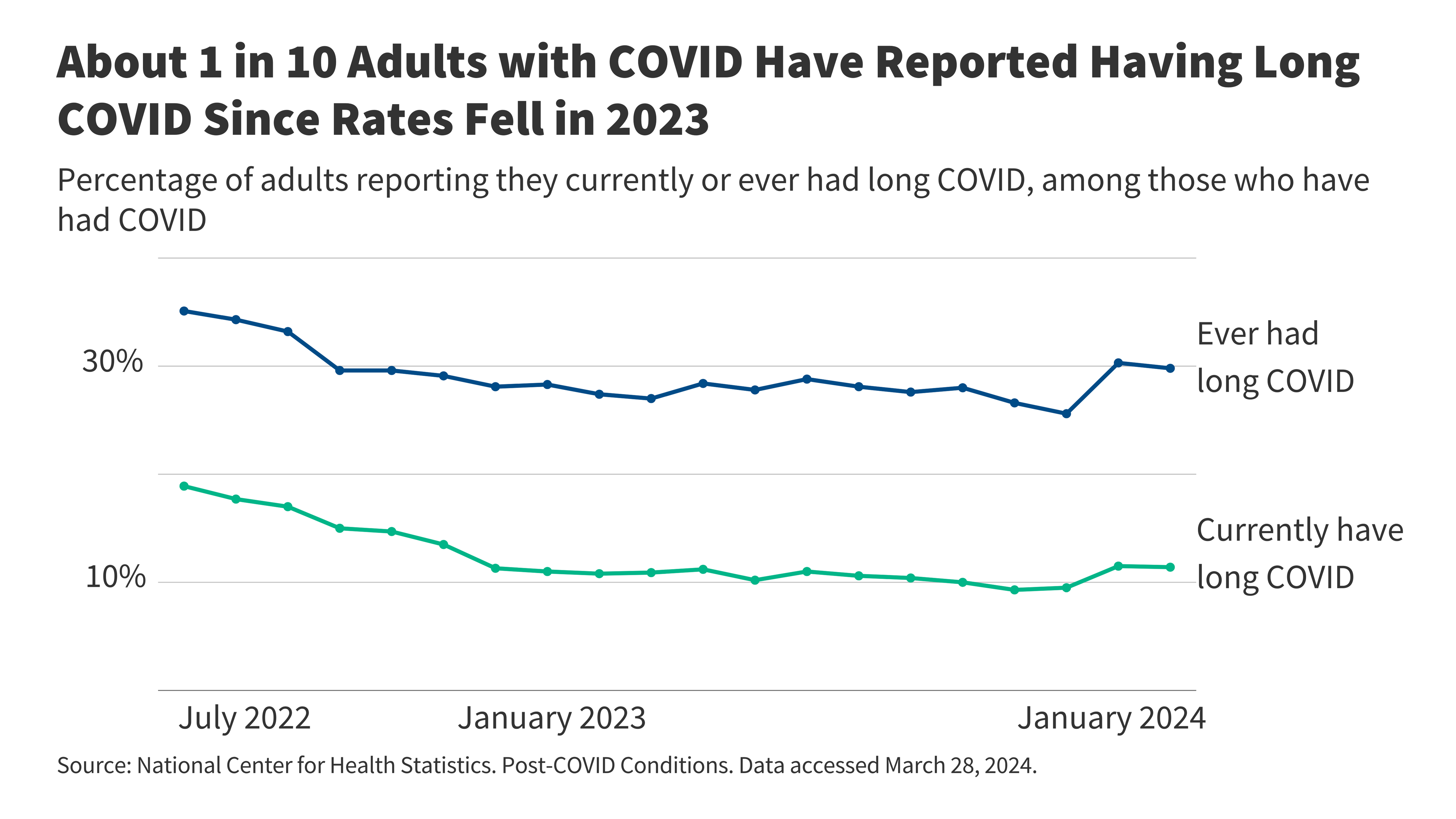
Among the 60% of U.S. adults who have had COVID, roughly 3 in 10 report having long COVID at some point and roughly 1 in 10 report having long COVID now (Figure 1). When the CDC first started asking about long COVID on the Household Pulse Survey, over one third of adults who had COVID reported having had long COVID. That percentage decreased through October 2023 but rose again in February 2024, nearing three in ten. At any point in time, a smaller percentage of adults currently have long COVID. Since December 2022, in any given month, roughly 10% of adults who have had COVID report having long COVID. The gap between the percent of adults who have long COVID now and the percent who ever have highlights that people are recovering.
An estimated 17 million adults currently have long COVID. There are roughly 250 million adults in the U.S. population, 43 million of whom report ever having had long COVID and 27 million of whom report having had it in the past but not having it currently. Those numbers are on par with the number of people who have cancer (17 million in 2020) and almost as many as the number with coronary artery disease (over 20 million in 2023). Those numbers are all based on self-reported data from the Household Pulse Survey, as reported by the CDC. The Pulse survey is an experimental survey providing information about how the COVID pandemic is affecting households from social and economic perspectives. Its primary advantage is the short turn-around time, but the data may not meet all Census Bureau quality standards. The percentage of people who self-report having had COVID in the survey may differ from rates of COVID from other data sources.
Among adults with long COVID, 79% report having any activity limitations from long COVID and 25% report that long COVID limits their activities “a lot” (Figure 2). The Pulse survey asks adults who report having long COVID whether it limits their day-to-day activities “a lot,” “a little,” or “not at all,” and characterizes the “a lot” responses as “significant.” Most people report activity limitations, but only one in four report long COVID limits their activities a lot. These numbers have changed little since the Pulse survey first started asking about activity limitations in September 2022. It is uncertain how well Pulse respondents represent all U.S. adults. On the one hand, it may be difficult for people with severe limitations to respond to the survey, so the survey may undercount with severe limitations. On the other hand, people who experience long COVID and especially, limitations from long COVID, may be more likely to respond to the survey, so the survey may overcount people those with activity limitations. Understanding the severity of limitations and whether they are permanent is relevant to the uncertainty surrounding how long COVID will affect employment and social engagement. Research has shown lower employment rates among adults with long COVID and although there is still uncertainty about the magnitude of the effects, recent work suggests that the net reduction in the labor force stemming from long COVID is equivalent to about one million workers.
Long COVID is most common among adults who are transgender or who have disabilities, groups that already experience greater difficulties in accessing health care (Figure 3). KFF’s analysis of earlier data on long COVID found higher rates of long COVID among adults who were Hispanic or Latino and those with lower levels of education, which raised questions as to whether long COVID would exacerbate existing disparities in health and employment. As more time has passed—and most adults in the U.S. have now contracted the virus at least once—rates of long COVID show less variation across groups based on race, ethnicity, and educational attainment, although people who are Asian and Black have lower rates of long COVID than those who are White and those who are Hispanic or Latino; and women have higher rates of long COVID than men. There are two groups with notably higher rates of long COVID than others, which include:
- People who are transgender (11% of whom have long COVID), and
- Adults with disabilities (12% compared of whom have long COVID).
People who are transgender and those with disabilities already face barriers accessing health care—which may contribute to their higher rates of long COVID—but higher rates of long COVID among such groups may also exacerbate such barriers.
Looking ahead, 5% to 10% of adults in the U.S. may continue to experience long COVID at any point in time, but research to improve diagnosis and treatment moves slowly. Although rates of long COVID have stabilized, the 17 million adults with long COVID may experience many employment and material hardships with 4 in 10 reporting food insecurity, 2 in 10 reporting difficulty paying rent or mortgage, and 1 in 10 reporting that they had to stop working for a period of time because of their symptoms. Patients testified about their challenges at a Senate Committee on Health, Education, Labor & Pensions hearing in January 2024, along with leading doctors researching long COVID. The witnesses called for additional federal funding to improve the diagnosis and treatment of long COVID but currently, most federal funding goes through the RECOVER initiative, which has been criticized for the way money was spent and the lack of meaningful breakthroughs. As of spring 2023, the federal government had spent $1 billion on the RECOVER initiative and still not signed up a single patient to test any treatments. In February 2024, the Biden Administration dedicated an additional $515 million to the same project. Despite challenges to the RECOVER initiative, researchers recently announced that they are closer to understanding the causes of long COVID, which may allow for improved ways to test for and treat it.
As society moves beyond the pandemic and COVID is increasingly treated as another respiratory virus, groups that are disproportionately more affected by long COVID, may find existing challenges accessing health care to be exacerbated. People with long COVID report statistically higher rates of challenges in accessing and affording health care. The groups with the highest rates of long COVID—adults who are transgender and those with disabilities—also have greater challenges accessing health care even without long COVID and experience higher rates of discrimination by providers. For example, a KFF/Washington Post survey of trans adults found that they had significant issues accessing health care, with nearly half reporting that it was difficult to find a health care provider with whom they could get an appointment with quickly and about half reporting that affordable health care was difficult to find. Beyond difficulties access care, trans adults reported multifaceted discrimination with 17% reporting that they had been denied health care from a provider because of their gender identify. People with disabilities also experience higher rates of discrimination and challenges accessing timely and comprehensive health care, which spurred the National Institutes of Health to designate people with disabilities as a population with health disparities for research purposes in September 2023. Such challenges likely contribute to higher rates of long COVID among adults who are transgender or have disabilities, but also exacerbate the challenges patients experience.

av8vl2
Thinker Pedia I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
Thinker Pedia I appreciate you sharing this blog post. Thanks Again. Cool.
fyg8el
had4co
nixfcp
Hi my family member! I want to say that this post is awesome, nice written and come with approximately all significant infos. I would like to peer extra posts like this.
hello!,I really like your writing so a lot! share we keep up a correspondence extra approximately your post on AOL? I need an expert in this house to unravel my problem. May be that is you! Taking a look ahead to see you.
4ckujs
aelosa
esjez5
w8vr7e
I do trust all the ideas you’ve presented in your post. They are really convincing and will definitely work. Nonetheless, the posts are too short for newbies. May just you please lengthen them a bit from next time? Thank you for the post.
ns4vlh
Thinker Pedia I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
zj29ak
I’ve read several just right stuff here. Certainly price bookmarking for revisiting. I wonder how a lot effort you place to create this kind of great informative website.
nf9z2t
4q8jgx
3culj1
zxv6k8
1g49mw
cukduh