Individuals who have asymptomatic COVID-19 may develop post-COVID conditions. These conditions can present as different types and combinations of health problems for different lengths of time, according to the US Centers for Disease Control and Prevention (CDC).1 Known as long-COVID, many patients exhibit a constellation of pain conditions. The most common long-COVID complaints include difficulty breathing, shortness of breath, tiredness, fatigue, postexertional malaise, chest pain, stomach pain, headache, heart palpitations, and musculoskeletal pain.
“The pain management is not yet standardized and should target symptoms. Multimodal approaches should be proposed and these encompass drug therapy, such as drugs that act on pain modulation, such as duloxetine, gabapentin, and pregabalin, with some precautions,” said pain management specialist and neurologist Nadine Attal, MD, PhD, from the Hôpital Ambroise Paré, Boulogne-Billancourt, France.
Physical therapy and psychological approaches also may be highly beneficial. Dr Attal and her colleagues conducted a review analyzing the most common viral infections responsible for neurological complications, including neuropathic pain.2 Neurological complications of COVID-19 were included, in particular Guillain-Barré syndrome, myelitis, and stroke in regard to their potential risk of chronic neuropathic pain. 2
Continue Reading
Dr Attal said the most commonly noted post-COVID pain complaint is widespread pain, which is often accompanied by fatigue, sleep disorders, and respiratory disorders. “This has been found repeatedly after other viruses, such as Epstein Barr Virus. However, it may be worse here because anatomical cadaver studies have shown that the virus spreads everywhere, including the brain,” Dr Attal indicated.
However, it is theorized that COVID-related pain symptoms are distinct from potential sequalea after direct COVID-19 neurological lesion, such as with Guillain-Barré Syndrome and myelitis, because these cases have only occurred in patients with very severe COVID-related problems. Dr Attal said all patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) should be followed closely. “[Healthcare providers] should not neglect these patients, and consider that many problems might be due to persisting viral infection and/or postviral immune reaction, and not solely psychological consequences,” Dr Attal said. “One important message is never use opioids and treat as fibromyalgia or neuropathic pain.”
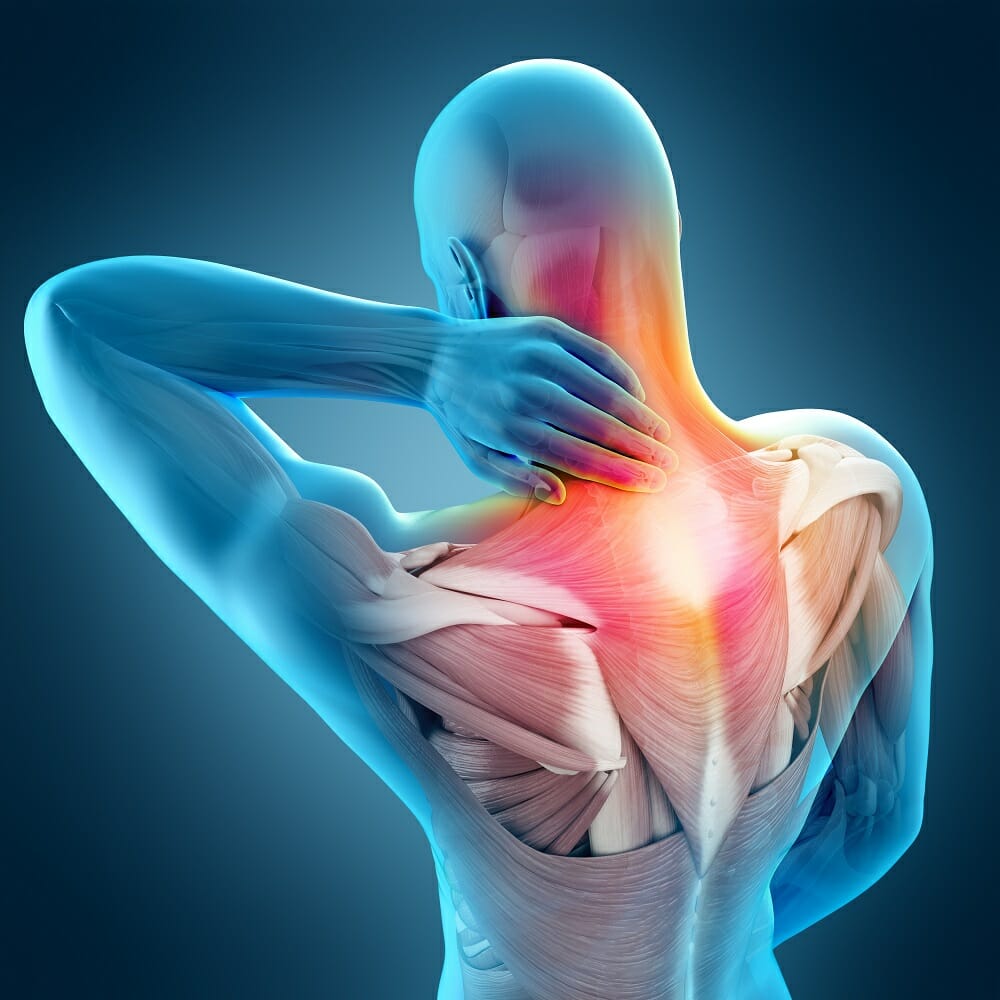
Mohab Ibrahim, MD, PhD, medical director of the University of Arizona Health Sciences Comprehensive Pain and Addiction Center and the director of the Chronic Pain Management Clinic, in Tucson, Arizona, said he is seeing mostly diffuse muscle and joint pain. However, less common pain complaints have included headache and neuropathic pain. “Just like any other pain presentation, consider developing a differential of possible etiologies for the patient. People with COVID-19 can still develop pain conditions, just like any other person before the COVID-19 pandemic. If other possibilities have been ruled out, keep in mind long-COVID is a multifactorial syndrome or disease,” Dr Ibrahim noted.
There still is little known about the long-term effects of COVID-19. However, many conditions can exacerbate pain following COVID-19 infection. Dr Ibrahim said many of his patients report sleep disturbances, depression, and anxiety in addition to pain. “These conditions can worsen and even prolong pain conditions. So, patients with long-COVID pain may benefit from a multimodal approach using pharmacological, such as nonsteroidal anti-inflammatory drugs, steroids, and antibiotics,” Dr Ibrahim commented.
Other nonpharmacological approaches like physical therapy, meditation, acupuncture, psychiatric support to address depression and anxiety, and interventional pain management may be highly beneficial.
Some of the possible reasons for pain associated with long-COVID include residual infection, prolonged immune response, organ damage or injury, and neuropathic pain. Hemant Kalia MD, MPH, interventional pain & cancer rehabilitation specialist at Rochester Regional Health in New York, said about 30% of symptomatic and 5% of patients with asymptomatic COVID-19 will continue to have proinflammatory cytokine-chemokine profile. “Although we don’t know the exact prevalence or incidence rates of chronic pain in these individuals, most of them complain of diffuse myofascial pain associated with fatigue, orthostatic intolerance, elevated heart rate, and poor sleep hygiene. Most of these symptoms can be attributed to excessive sympathetic nervous system activity,” Dr Kalia added.
There is a predisposition of worsening chronic pain syndromes in those infected with COVID-19 and already suffering from an underlying diffuse inflammatory response, such as fibromyalgia. “There are case reports3 elucidating benefits from interventions like stellate ganglion nerve block, which is a nerve bundle in the neck, that is responsible for modulating sympathetic outflow,” said Dr. Kalia.
At his institution, the team has treated 4 patients with this approach (3 of them were acute COVID-19 patients and 1 met the criteria for long-COVID syndrome with myofascial pain). “We can certainly speculate why some of these patients continue to report a constellation of symptoms including fatigue and chronic pain but unfortunately, we don’t have enough epidemiological studies to ascertain cause and effect relationship and its subsequent burden on the population” said Dr. Kalia.
Zayad Al-Aly, MD, director of the Clinical Epidemiology Center, and chief of the Research and Education Service at the Veterans Affairs Saint Louis Health Care System in Missouri, said pain is one of the main sequelae of long-COVID, yet there is no formal name for the constellation of symptoms. “Because [patients with Long-COVID] generally complain of pain in multiple sites, some people are using the term ‘multisite’ pain. There is no agreed upon standardized terminology for pain in long-COVID,” Dr. Al-Aly said.
With a lack of consensus for a name and no guidance yet on treatment approaches, Dr All-Aly said action is required to mitigate the risk of larger problems in the future. “I think the important thing to point out is that we see evidence of increased risk of opioid prescribing in people with COVID-19 and long-COVID. This is happening at high rates and demands urgent attention. Pain should be treated, but opioids should be used as medications of last resort. I worry that the increased use of opioids in people with long-COVID might balloon to a much larger crisis down the road,” Dr All-Aly noted.
References
1. Centers for Disease Control and Prevention (CDC). Post-COVID conditions. Updated September 16, 2021. Accessed January 19, 2022. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
2. Attal N, Martinez V, Bouhassira D. Potential for increased prevalence of neuropathic pain after the COVID-19 pandemic. Pain Rep. Published online January 27, 2021. doi:10.1097/PR9.0000000000000884
3. Liu LD, Duricka DL. Stellate ganglion block reduces symptoms of Long COVID: A case series. Journal of Neuroimmunology. 2022;362:577784
This article originally appeared on Clinical Pain Advisor
this content first appear on medical bag