A 65-year-old woman presents to the emergency department with complaints of shortness of breath, sore throat, fever, chills, productive cough, and substernal chest pain. She tested positive for COVID-19 six days earlier.
On initial presentation, her oxygen saturation is 90% on room air and chest radiography reveals diffuse bilateral alveolar infiltrates and prominent vascular congestion. A 12-lead electrocardiogram (ECG) reveals anterior ST elevation with deep anterior T-wave inversion. Results of inflammatory markers and laboratory tests are shown in Table 1.
Table 1. Inflammatory Markers and Laboratory Test Results
| Test | Result |
| BNP, pg/mL | 790 |
| C-reactive protein, mg/L | >300 |
| D-dimer, µg/mL | 2.184 |
| Ferritin, ng/mL | 320 |
| Interleukin 6, pg/nL | 724.38 |
| Troponin I, ng/mL | 0.90 |
Significant Medical History
Medical history is significant for hypertension, hypothyroidism, glaucoma, and generalized anxiety disorder. Medication management includes lisinopril 10 mg daily, latanoprost ophthalmic solution for both eyes daily, and citalopram 20 mg daily.
Continue Reading
Physical Examination
The patient is a middle-aged woman with obesity in moderate respiratory distress. Admission vital signs include blood pressure 96/52 mm Hg, heart rate 107 beats per minute, and respiratory rate 28 breaths per minute. Her oxygen saturation improves to 94% with initiation of 4 L/min oxygen via nasal cannula. Pulmonary examination reveals mild expiratory wheezing. No murmurs or extra heart tones are noted on cardiac auscultation. Mild jugular venous distention is observed.
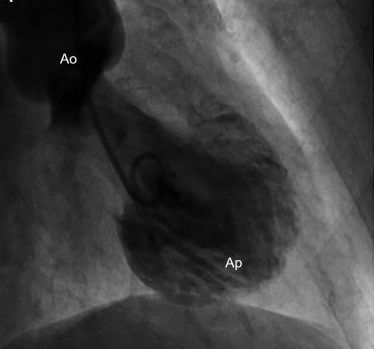
After occlusive coronary disease was ruled out with angiography, she was diagnosed with Takotsubo syndrome (TTS).
Discussion
Takotsubo syndrome is thought to be precipitated by severe emotional or physical stress, likely mediated by catecholamine surge leading to myocardial stunning.1 Takotsubo syndrome is most commonly diagnosed in postmenopausal, White women. Pathophysiology of TTS has been theorized to be secondary to a systemic inflammatory response,2 endothelial dysfunction leading to impaired myocardial perfusion, and myocardial stunning,1 as well as a form of microvascular acute myocardial infarction.1-3 Although most patients (95%) fully recover from TTS, the in-hospital mortality risk is estimated to be 5%.4
A marked increase in the incidence of TTS has occurred since the start of the COVID-19 pandemic.5,6 Prior to the global pandemic, the incidence of TTS in patients presenting with acute coronary syndrome was between 1.5% and 1.8%.5 One study found the incidence of TTS during the COVID-19 pandemic to be as high as 7.8%.5 Although several case reports of concurrent COVID-19 infection and TTS can be found in the literature, a significant increase in the number of cases of TTS without concurrent COVID-19 infection also has been observed.6 Proposed mechanisms for the increased incidence of TTS in the general population during the pandemic include worsened anxiety, panic, and depression levels in the public secondary to the psychological distress from the pandemic.
Diagnosis
Most patients presenting with TTS complain of chest pain and dyspnea and have an ECG presentation of ST-segment elevation myocardial infarction (STEMI): increased cardiac biomarkers, left ventricular (LV) dyskinesia, and in most cases some recent physical or emotional trigger.3,4 Diagnosis of TTS is made when acute myocardial infarction is suspected with no angiographic evidence of coronary blockage and 4 of the Revised Mayo Clinic Criteria for Takotsubo cardiomyopathy are met4:
- Transient dyskinesia of the left ventricle midsegments; regional wall motion abnormalities beyond a single epicardial vascular distribution
- Absence of obstructive coronary artery disease or acute plaque rupture
- New ECG abnormalities or modest troponin elevation
- Absence of pheochromocytoma and myocarditis
Table 2. Recommended Diagnostic/Laboratory Tests for Takotsubo Syndrome3,7,8
| Troponin, BNP |
| 12-lead ECG |
| Coronary angiography |
| Echocardiography |
Laboratory Studies
Troponin levels are increased in most cases of TTS and brain-type natriuretic peptide (BNP) level is markedly elevated.3
12-Lead ECG
The 12-lead ECG may show evidence of ST-segment elevation or ST-segment depression3; ST-segment elevation in 2 or more contiguous leads is diagnostic for STEMI.8 Patients with TTS may show anterior ST elevation with deep anterior T-wave inversion.7
Coronary Angiography
The American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines recommend emergent coronary angiogram in the setting of chest pain, elevated biomarkers, and ST-segment elevation on a 12-lead ECG.7,8 Coronary angiography is diagnostic for underlying coronary disease and can identify precise lesions precipitating coronary injury.8 If culprit lesions are identified, a reperfusion strategy can be initiated. Patients with TTS will have no evidence of obstructive coronary disease on angiography.4,7 Data regarding intracardiac pressures, valvular function, and structural impairments can also be identified with angiography. A left ventriculogram can provide information about LV systolic function. Coronary angiogram is currently the definitive tool for differentiating TTS from acute coronary syndrome.7
Transthoracic Echocardiogram
Transthoracic echocardiogram will demonstrate LV wall-motion abnormalities and can rule in or rule out LV outflow tract obstruction (LVOTO).7 Transthoracic echocardiogram is also used for evaluation of LV thrombus.7
Management and Treatment
Treatment for TTS includes supportive care and management of complications such as shock, heart failure, and LV thrombus.6 Case severity can range from mild, which may not need intervention, to severe, which may require aggressive intervention.7 Management recommendations are divided into 4 categories:
1. Takotsubo Syndrome Without Complications
Treatment for TTS is mainly supportive until LV function spontaneously improves.4,6,7 Improvements in LV function usually occur within 21 days of symptom onset with most patients fully recovering within 2 months.4,6 Treatment is typically provided for up to 3 months and may include dual antiplatelet therapy, anticoagulants for patients with large areas of cardiac hypokinesis, beta-blockers, angiotensin-converting enzymes inhibitors (ACEI) or angiotensin receptor blockers (ARB), statins, and stress relief management.7
2. Takotsubo Syndrome With Hypotension and Cardiogenic Shock
In patients who have TTS with hypotension and cardiogenic shock, continuous monitoring of vital signs and end-organ perfusion are required.7 Careful administration of fluids can be performed in patients not exhibiting manifestations of pulmonary congestion.7 Positive inotropes, such as dobutamine or dopamine, and/or vasopressor infusions can serve as a temporary measure in cases of cardiogenic shock without LVOTO.7 Positive inotropes and vasopressors can increase the degree of obstruction in cases of moderate to severe LVOTO and are therefore contraindicated.4,7 The alpha agonist phenylephrine can be used cautiously in cases of LVOTO. Patients who have persistent hypotension despite initial measures may need mechanical circulatory support devices such as the intra-aortic balloon pump or extracorporeal membrane oxygenation.7
3. Takotsubo Syndrome With Heart Failure
Except in cases of LVOTO, standard heart failure management is recommended.7 This includes management of oxygenation and ventilation along with preload and afterload reduction.7 Standard heart failure medications are used such as diuretics and ACEI/ARBs.7 In cases of heart failure with LVOTO, standard preload and afterload reduction therapies should be avoided.7
4. Takotsubo Syndrome With Thromboembolism
Patients with severe LV dysfunction are at increased risk for ventricular thrombus development. In cases of severe LV dysfunction but no thrombus and low bleeding risk, anticoagulation is indicated until akinesia or dyskinesia is resolved or for 3 months, whichever is shorter.7 In the presence of ventricular thrombus, anticoagulation is indicated for 3 months with the duration of treatment modified based on rate of recovery of cardiac function and resolution of thrombus.7
Discussion/Follow-Up
Duration of treatment for TTS generally ranges from 3 months to 1 year and will be determined based on return of cardiac function. Patients with TTS who experience complications such as cardiogenic shock, heart failure, or thromboembolism may require long-term care. Frequent assessments using serial echocardiography will be needed to check recovery of cardiac function in these patients. Fortunately, most patients fully recover within weeks.4,7
Frances Stueben, DNP, RN, CHSE, is an assistant professor and simulation program coordinator at the University of Louisiana at Lafayette. She teaches in the graduate and undergraduate nursing programs.
Deedra Harrington, DNP, MSN, APRN, ACNP-BC, is associate professor at the College of Nurse and Allied Health Professions, University of Louisiana at Lafayette. Dr Harrington is an advanced practice registered nurse-acute care who works with an inpatient cardiology intensivist group in Louisiana.
Christy L. McDonald Lenahan, DNP, FNP-BC, ENP-C, CNE, is an advanced practice registered nurse in family and emergency medicine who works for an emergency medicine and hospitalist staffing agency. She is also an associate professor at the University of Louisiana at Lafayette and teaches in the masters and doctoral programs.
Links to other articles in this series:
1. Management of NSTEMI/STEMI in patients with COVID-19, click here
2. Venous thromboembolism management in patients with COVID-19, click here
3. Atrial fibrillation and other dysrhythmias in patients with COVID-19, click here
4. Acute pericarditis, myopericarditis, and perimyocarditis in patients with COVID-19, click here
5. Heart failure in patients with COVID-19, click here
6. Cardiogenic shock in patients with COVID-19, click here
References
- Chiu S, Nayak R, Lin B, Duan L, Shen AY, Lee MS. Clinical characteristics and outcomes of patients with Takotsubo syndrome. Can J Cardiol. 2021;37(8):1191-1197. doi:10.1016/j.cjca.2021.01.014
- Ruzzenenti G, Maloberti A, Giani V, et al; COVID-19 Niguarda Working Group. COVID and cardiovascular diseases: direct and indirect damages and future perspective. High Blood Press Cardiovasc Prev. 2021;28(5):439-445. doi:10.1007/s40292-021-00464-8
- Lüscher TF, Templin C. Is Takotsubo syndrome a microvascular acute coronary syndrome? Towards of a new definition. Eur Heart J. 2016 Oct 1;37(37):2816-2820. doi: 10.1093/eurheartj/ehw057
- Boyd B, Solh T. Takotsubo cardiomyopathy: review of broken heart syndrome. JAAPA. 2020;33(3):24-29. doi:10.1097/01.JAA.0000654368.35241.fc
- Jabri A, Kalra A, Kumar A, et al. Incidence of stress cardiomyopathy during the Coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(7):e2014780. doi:10.1001/jamanetworkopen.2020.14780
- Shah RM, Shah M, Shah S, Li A, Jauhar S. Takotsubo syndrome and COVID-19: associations and implications. Curr Probl Cardiol. 2021;46(3):100763. doi:10.1016/j.cpcardiol.2020.100763
- Sattar Y, Siew KSW, Connerney M, Ullah W, Alraies MC. Management of Takotsubo syndrome: a comprehensive review. Cureus. 2020;12(1):e6556. doi:10.7759/cureus.6556
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78-e140. doi:10.1016/j.jacc.2012.11.019
This article originally appeared on Clinical Advisor
this content first appear on medical bag