The public health and economic effects of the pandemic continue to affect the well-being of many Americans. The American Rescue Plan included funding not only to address the public health crisis of the pandemic, but also to provide economic support to many low-income people struggling to make ends meet. Millions have lost jobs or income since the start of the pandemic, making it difficult to pay expenses including basic needs like food and housing. These challenges will ultimately affect people’s health and well-being, as they influence social determinants of health. This brief provides an overview of social determinants of health and a look at how adults are faring across an array of measures as of September 2021 when a portion of the population remained unvaccinated, and hospitalizations and deaths due to the delta variant are surging in some areas even as they wane in others.
What are social determinants of health?
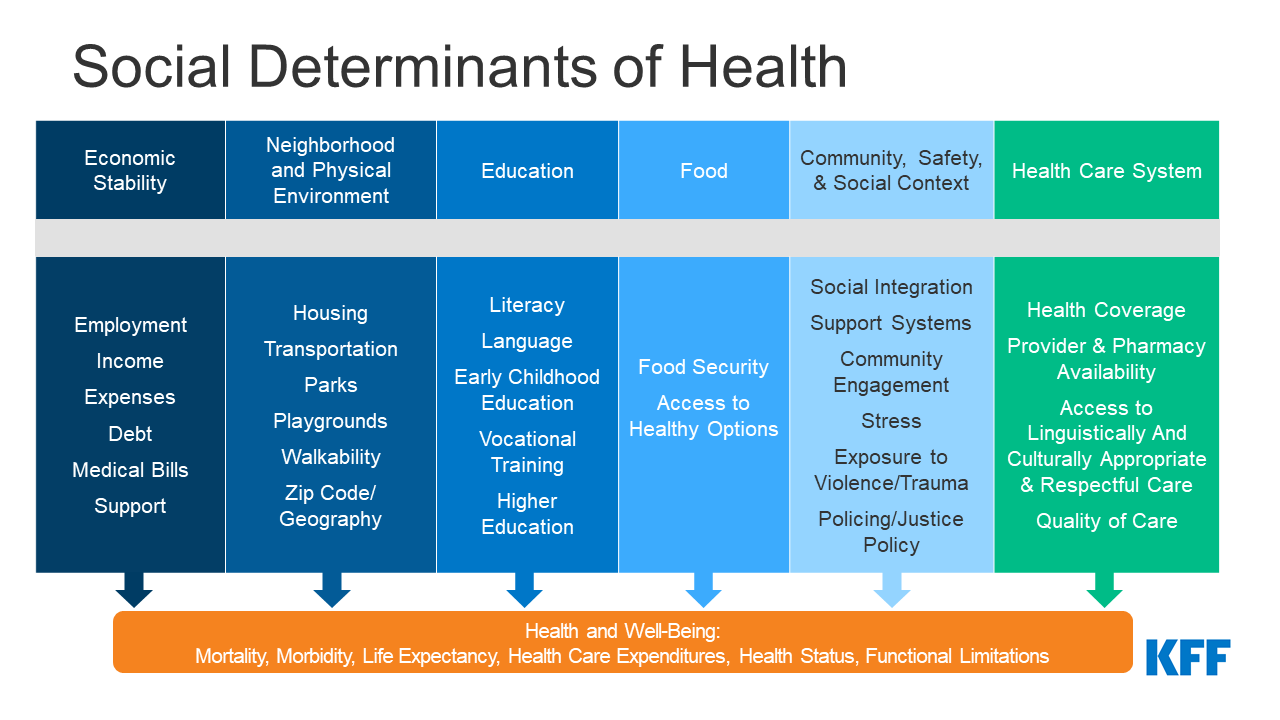
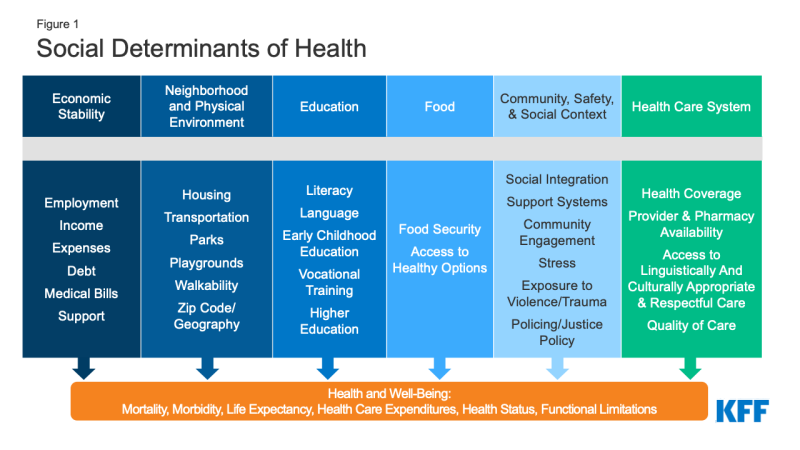
Social determinants of health are the conditions in which people are born, grow, live, work, and age. They include factors like socioeconomic status, education, neighborhood and physical environment, employment, and social support networks, as well as access to health care (Figure 1).
Though health care is essential to health, research shows that health outcomes are driven by an array of factors, including underlying genetics, health behaviors, social and environmental factors, and financial distress and all of its implications. While there is currently no consensus in the research on the magnitude of the relative contributions of each of these factors to health, studies suggest that health behaviors and social and economic factors are the primary drivers of health outcomes, and social and economic factors can shape individuals’ health behaviors. There is extensive research that concludes that addressing social determinants of health is important for improving health outcomes and reducing health disparities. Prior to the pandemic there were a variety of initiatives to address social determinants of health both in health and non-health sectors. The COVID-19 pandemic exacerbated already existing health disparities for a broad range of populations, but specifically for people of color.
How are adults faring across a range of social determinants of health during the pandemic?
Across a wide range of metrics, large shares of people are experiencing hardship. The Census Bureau’s Household Pulse Survey was designed to quickly and efficiently collect and compile data about how people’s lives have been impacted by the coronavirus pandemic. For this analysis we looked at a range of measures over the course of the pandemic. Unfortunately, the Household Pulse Survey does not provide pre-pandemic measures for comparison. While we have tracked data over time and there have been fluctuations at various points since March 2020, patterns of hardship remain largely consistent, and changes in measures do not necessarily follow economic indicators or pandemic trends. Data for the most recent period, September 1 – September 13, show that (Figure 2):
- More than one in six adults (17.4%) reported that they or someone in their household had experienced a loss of employment income in the past four weeks;
- More than half (50.9%) of adults reported difficulty paying for usual household expenses in the past 7 days, and 30.5% used credit cards or loans to meet household spending needs;
- 5% of adults had no confidence in their ability to make next month’s housing payment (across renters and owners), and 8.8% reported food insufficiency in their household;
- Nearly one in three (32.1%) adults reported symptoms of depression or anxiety.
Black and Hispanic adults fare worse than White adults across nearly all measures, with large differences in some measures. In September 2021, nearly seven in ten of Black and Hispanic adults (66.4% and 69.2%, respectively) reported difficulty paying household expenditures compared to 43.6% of White adults; 12.9% of Black adults and 10.6% of Hispanic adults reported no confidence in their ability to make next month’s housing payment compared to 4.1% of White adults; and 14.9% of Black adults and 14.2% of Hispanic adults reported food insufficiency in the household compared to 6.3% of White adults. Furthermore, around a quarter of Black and Hispanic adults reported living in a household that experienced a loss of employment income in the last four weeks (24.9% and 27.2%, respectively) compared to 13.1% of White adults.
While variation across age and gender was not as stark, younger adults (ages 18 to 44) fared worse on many measures compared to older adults. For example, higher shares of younger adults reported symptoms of anxiety and depression as well as difficulty paying for usual household expenses. In addition, higher shares of women reported symptoms of depression or anxiety and difficulty paying usual household expenses in the past seven days compared to men.
Across most measures, adults with children in their household fared worse compared to overall adults. For example, 22.0% of adults with children in the household experienced loss of employment income in the household in the last four weeks compared to 17.4% of adults overall, and six in ten (59.7%) adults with children in the household reported difficulty paying for household expenses in the past week compared to the overall population of 50.9%. Adults in households with children were also more likely to report food insufficiency, symptoms of depression or anxiety, and no confidence in ability to make next month’s housing payment than the general population.
Patterns of hardship over time indicate both effects of the pandemic and related policies as well as longstanding disparities in social determinants of health. Data indicate the shares of people experiencing hardships peaked in December 2020 but have otherwise remained largely stable (Figure 2). Trends across all measures have improved since December 2020, reaching lows during the pandemic in March and April 2021, likely reflecting the roll-out of the COVID-19 vaccines and new federal funding available during that period. However, differences in rates of hardship among certain populations has remained largely stable throughout the pandemic and to some extent reflect longstanding disparities that existed even before the pandemic. Still, understanding these disparities in the context of heightened levels of need over the past year highlights these differences and who may benefit most from government assistance.
What to watch going forward
The American Rescue Plan provides $1.9 trillion in funding to address the ongoing health and economic effects of the pandemic. Some of the provisions that provide key economic support for individuals include direct stimulus payments to individuals, an extension of federal unemployment insurance payments, a child tax credit of up to $300 per child per month from July through the end of the year, additional funding to address food insecurity, emergency rental assistance, and emergency housing vouchers. This federal support may have contributed to some improvements in metrics, but hardship is also affected by the trajectory of the pandemic (including a surge in cases and deaths due to the delta variant and any changes in vaccination rates). Looking ahead, the effects of some temporary federal support and the pandemic are likely to continue to be factors in future data releases; however, additional and extended federal support being debated in Congress that may seek to address underlying economic issues beyond the pandemic has the potential to change long-standing patterns of hardship across different demographic groups.