There are approximately 48 million children under the age of 12 in the United States. This group is not yet eligible for COVID-19 vaccination, though it is widely expected that a vaccine will be authorized for at least some children by the end of the year (clinical trials are currently underway among children between the ages of 6 months and 11 years old). Although children have not borne the most severe brunt of COVID-19 relative to adults, some do become hospitalized, suffer long-term consequences, and even death from the disease. In addition, children can transmit to others, contributing to ongoing community transmission in the U.S., as the country continues to struggle to contain the virus in the midst of the much more transmissible Delta variant. Achieving a high rate of vaccine coverage among those under age 12, once eligible, is therefore important to protecting children and controlling continued spread of COVID-19, particularly as it is expected that many children will return to in-person schooling in the fall.
But reaching younger children may pose new challenges, including concerns about vaccination among parents. In almost all states, parental consent for vaccination is required for those under age 12. Yet, our KFF COVID-19 Vaccine Monitor surveys find that parents of younger children remain cautious about vaccinating their children against COVID-19, with almost three quarters (73%) saying they will either wait and see, will only do so if required by school, or won’t do so at all, although these views may change once a vaccine is authorized for kids. In addition, parents who may be willing to get their children vaccinated against COVID-19 could face barriers to accessing the vaccine.
Better understanding the characteristics of children under 12 in the U.S. may help inform vaccination efforts when they become eligible. We analyzed data from the U.S. Census and the 2019 American Community Survey to provide an overview of the population by age, region and state, race/ethnicity, poverty, and insurance status (see Methods for more information).
- There are 48 million children under the age of 12 in the United States, almost three times the number of adolescents, aged 12-15, the most recent age group to become eligible for COVID-19 vaccination. Over half are between the ages of 5 and 11 (59.2%), the subset for whom authorization of a vaccine may come next. A quarter (24.9%) are between the ages of 2-4 and the remainder (15.9%) are under the age of 2. (A COVID-19 vaccine is not being tested for those under the age of 6 months, but data were not available to disaggregate further by age).
- Children under the age of 12 represent 14.6% of the U.S. population, ranging from 11.6% in Maine to 19.5% in Utah. The largest share of children under age 12 live in the South (39.1%), followed by the West (24.3%), Midwest (21.0%), and Northeast (15.6%).
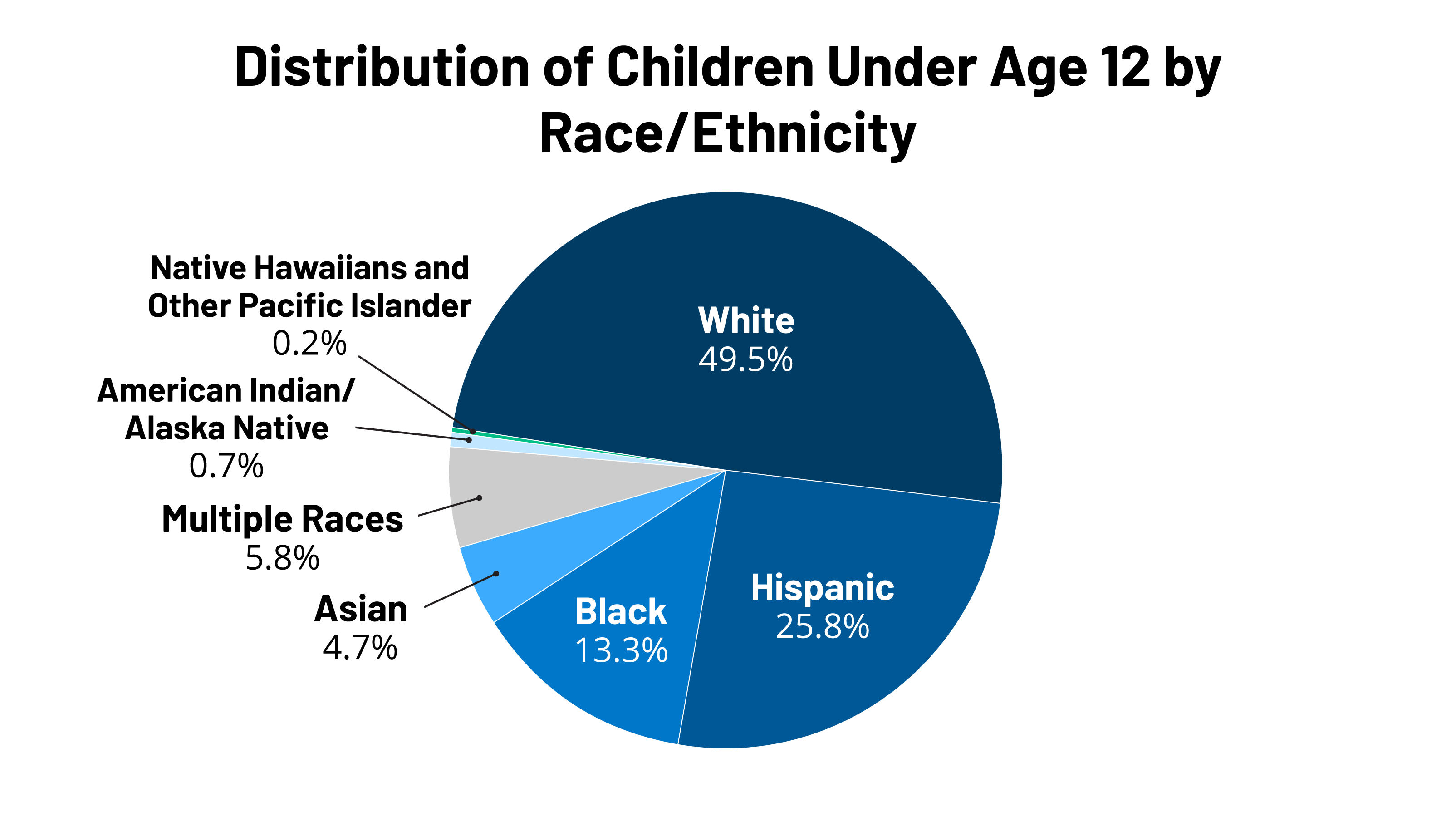
- About half (50.5%) of children under the age of 12 are children of color, including more than a quarter (25.8%) who are Hispanic. An additional 13.3% are Black, 4.7% are Asian, and the remaining 6.7% are American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, or multiracial (Figure 1). Some states have even larger shares of children of color. For example, in 5 states (Hawaii, New Mexico, the District of Columbia, California, and Texas), more than two-thirds of children under age 12 are children of color (Table 1). Over 4 in 10 children under age 12 are Hispanic in five states, including 60.4% in New Mexico and 52.0% in California. In 4 states, more than a third of children under age 12 are Black including 48.5% of children in DC and 42.8% of children in Mississippi. Over 1 in 10 children under age 12 are Asian in California (11.1%) and this share rises to nearly a quarter (22.6%) in Hawaii. Overall, children under age 12 include a larger share of people of color compared to the rest of the population (50.5% vs. 38.1%).
- Almost four in ten (39.4%) children under the age of 12 live in households with incomes below 200% of the Federal Poverty Level (FPL). This includes 17.5% living below poverty and 21.9% between 100-200% FPL. The remainder are split between households with incomes between 200-400% FPL (30.2%) and at or above 400% FPL (30.4%) (Figure 2). Some states have much higher shares of children living in low-income households, including 3 states with more than half of children under 12 living in households with incomes less than 200% FPL – Mississippi (53.3%), Arkansas (53.1%), and New Mexico (50.6%). In 13 states, more than one-fifth of children live below poverty (Table 2). Children under age 12 are more likely to be living in poverty compared to the rest of the population (17.5% v. 11.5%).
- Finally, while the majority of children under the age of 12 have health coverage, including 4 in 10 (39.8%) who are covered by Medicaid, 5.0% are uninsured (Figure 3). Because of broader Medicaid coverage, the uninsured rate for children under age 12 is nearly half that of those 12 and older (9.9%). Similar shares of children under age 12 and the rest of the population have private coverage.
Implications
Overall, these data show that children under age 12 account for a sizeable share of the population, suggesting that achieving a high vaccination rate among this group will not only be important for protecting them against infection and illness but can also help boost the country’s overall vaccination rate, facilitating efforts to contain the spread of the virus.
The data further show that children in this age group are more racially diverse than those older than age 12 and include a particularly high share of Hispanic children. They also are more likely than their older counterparts to be living in low-income or poor households. As such, success vaccinating this group may help to reduce racial disparities in overall vaccination rates for Black and Hispanic people. However, these data also highlight the importance of prioritizing equity when vaccinations begin for children under age 12 and focusing on reducing barriers to vaccination that disproportionately affect people of color and low-income people, such as concerns about missing work, transportation challenges, and/or other logistical barriers or information gaps.
Finally, an added challenge to vaccinating children in this age group is that a large share live in the South and in other states where vaccination rates are lowest. Direct outreach to parents in these states to address their questions and concerns about the vaccine will be important, as will working with pediatricians and family physicians to provide trusted information to parents and to administer vaccines. Schools will also likely play an important role in providing information and outreach to parents, and in some cases offering or requiring vaccination, particularly for those parents who say they want to wait and see or will only vaccinate their child if schools require it.
| Methods |
| Population totals are all sourced from the Census Bureau’s 2019 Population Estimates: Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States: April 1, 2010 to July 1, 2019 (NC-EST2019-AGESEX-RES), available here: https://www.census.gov/data/tables/time-series/demo/popest/2010s-national-detail.html. Demographic, insurance, and geographic measures are sourced from KFF’s analysis of the 2019 American Community Survey (ACS), 1-Year Estimates. The population totals using ACS total to 46.6 million under age 12. This difference is likely attributed to children having missing income-to-poverty ratios, which are needed to create households within the data. For more information on our methodology to create households within the ACS data, see: https://www.kff.org/report-section/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid-technical-appendix-a-household-construction/. |