Although the clinical features of SARS-CoV-2 infection were first reported in 2019, it has also been established that hospitalized patients with COVID-19, especially those admitted to intensive care unit (ICU), have an increased risk for venous thromboembolism (VTE) despite prophylactic dose anticoagulation.1-4 As a result, some experts have suggested that higher anticoagulation targets may be necessary for critically ill patients with COVID-19 pneumonia.5 An ongoing challenge in treating these patients is the absence of high-quality evidence to guide clinical decision-making.
In a review published in the International Journal of Environmental Research and Public Health, Christian Zanza, MD, PhD, of the department of emergency medicine at the Catholic University of Rome in Italy, and colleagues, summarized current literature surrounding the treatment of coagulation abnormalities in patients with COVID-19.5
Coagulation Abnormalities in COVID-19
Continue Reading
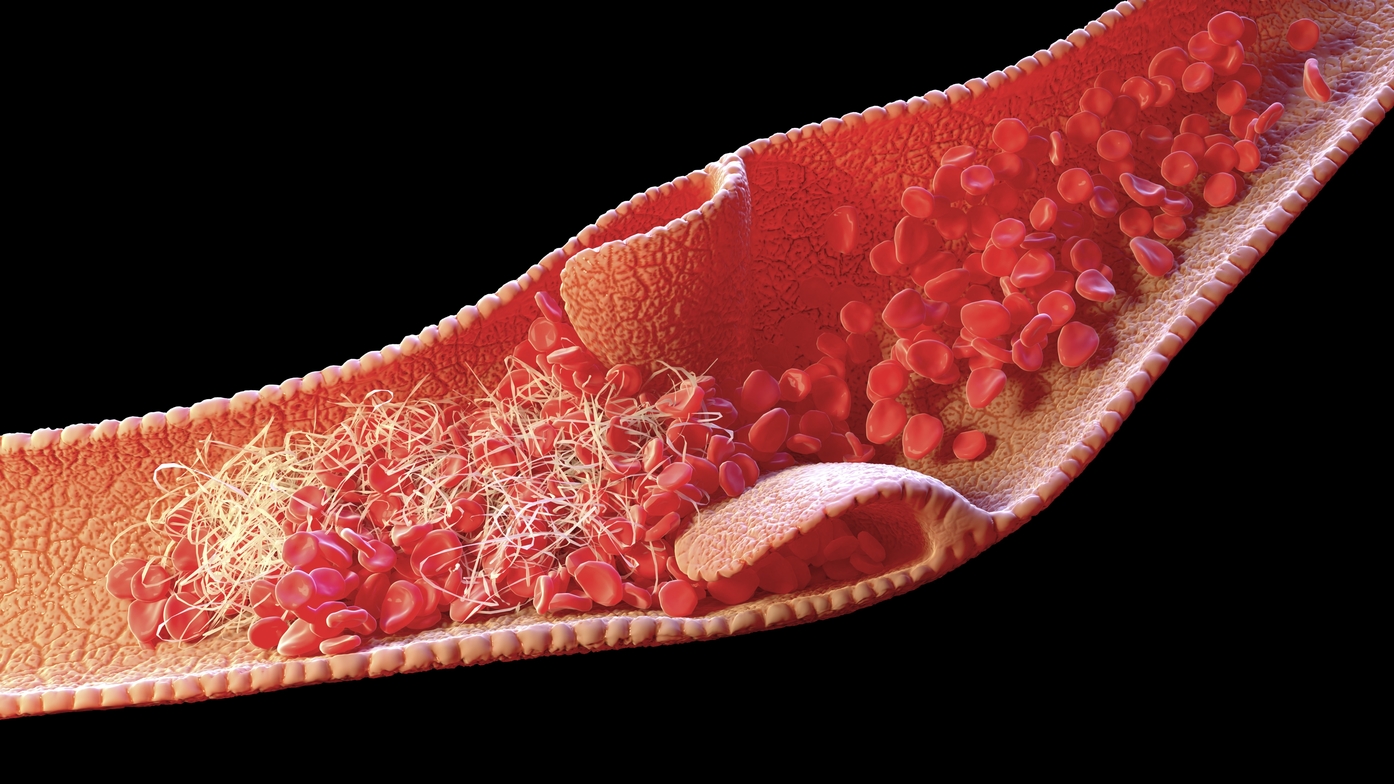
Infection with COVID-19 may predispose patients to both venous and arterial thrombotic events, thought to be the result of platelet activation, endothelial dysfunction, and hyperinflammation. Although bleeding is not commonly observed in patients, it may occur for other reasons, such as anticoagulation therapy or trauma, and if present, treatment consists of anticoagulant reversal or discontinuation, transfusions, or hemoderivatives for concurrent bleeding disorders. The presence of specific laboratory findings in COVID-19 may indicate a hypercoagulative state is present (Table 1).
| Table 1. List of laboratory findings indicative of a hypercoagulative state in COVID-195 |
| D-dimer elevated |
| Fibrinogen elevated |
| aPTT and PT normal or slightly prolonged |
| Platelet counts normal or increased |
| Factor VIII activity increased |
| VWF antigen greatly increased |
| Small decreases in antithrombin and small increases in protein C |
| Abbreviations: aPTT, activated partial thromboplastin time; PT, prothrombin time; VWF, von Willebrand factor |
Other laboratory findings include the presence of a lupus anticoagulant, which is common in those with prolonged aPTT. In addition, markedly elevated levels of D-dimer may correlate with illness severity, particularly if levels are increased several-fold.
Current evidence suggests the presence of a hypercoagulative state differs from disseminated intravascular coagulation (DIC); however, some patients with COVID-19 may also satisfy the criteria for probable DIC. Evidence of acute DIC includes increased plasma D-dimers, bleeding, thrombocytopenia, low plasma fibrinogen, prolonged aPTT and PT, and microangiopathic changes on peripheral blood smear.
The 2009 International Society of Thrombosis and Haemostasis (ISTH) scoring system may help diagnose DIC in patients with COVID-19 infection. For full details of the scoring system, readers should refer to the full publication in the International Journal of Environmental Research and Public Health.5
VTE in Patients With COVID-19
Critically ill and hospitalized patients with COVID-19 are at high risk for VTE primarily due to immobility, with pulmonary embolism (PE) being the most serious clinical manifestation of VTE. Clinical assessment for PE in these patients is challenging because the symptoms often overlap with COVID-19, and imaging studies may not be viable in all cases. The authors of this review recommended that the threshold for diagnosis of VTE should be low in patients with COVID-19.
With respect to anticoagulation, most medical societies still recommend using standard prophylactic dosing for hospitalized patients, but some physicians have advocated for empiric use of therapeutic anticoagulation, even in those without a documented diagnosis of VTE. Given the current state of evidence, the authors concluded that VTE prophylaxis with at least prophylactic dosing is appropriate in all hospitalized medical, surgical, and obstetric patients with COVID-19, unless there is a contraindication to anticoagulation, such as active or serious bleeding in the preceding 24 to 48 hours.
With respect to agent, low molecular weight heparin is preferred, but unfractionated heparin may also be used in patients with severe renal impairment. In cases of heparin-induced thrombocytopenia, an alternative therapy, such as fondaparinux, may be administered. In addition, therapeutic (full dose) anticoagulation for a minimum of three months is appropriate to treat VTE, and tissue plasminogen activator is suitable for massive PE, unless a contraindication is present.
Expert Perspective: The Importance of COVID-19 Vaccination
“It is very clear that COVID-19-related morbidity is substantial for patients with different malignant disorders, particularly in those with hematological malignancies,” commented Balazs Halmos, MD, of the department of medicine at the Albert Einstein College of Medicine in New York.
“Encouraging COVID-19 vaccinations amongst these patients is of paramount importance, and is strongly endorsed by all relevant agencies,” Dr Halmos further explained.
References
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-513. doi:10.1016/S0140-6736(20)30211-7
- Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094-1099. doi:10.1111/jth.14817
- Longhitano Y, Racca F, Zanza C, et al. Venous thrombo-embolism in hospitalized SARS-CoV-2 patients treated with three different anticoagulation protocols: prospective observational study. Biology. 2020;9(10):310. doi:10.3390/biology9100310
- Demelo-Rodríguez P, Cervilla-Muñoz E, Ordieres-Ortega L, et al. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thromb Res. 2020;192:23-26. doi:10.1016/j.thromres.2020.05.018
- Zanza C, Racca F, Longhitano Y, et al. Risk management and treatment of coagulation disorders related to COVID-19 infection. Int J Environ Res Public Health. 2021;18(3):1268. doi:10.3390/ijerph18031268.
This article originally appeared on Rheumatology Advisor
this content first appear on medical bag