Introduction
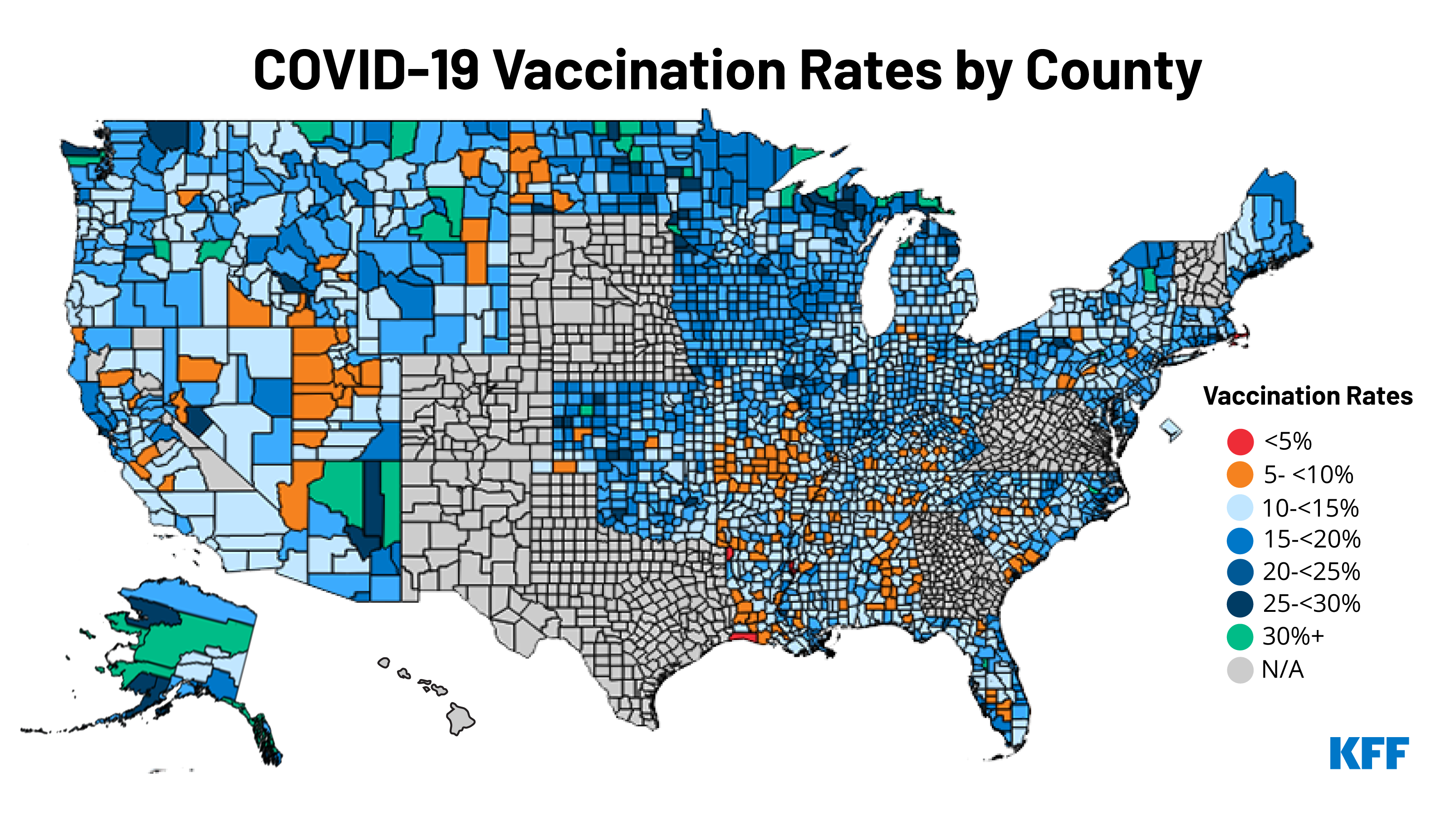
COVID-19 has disproportionately affected certain underserved and high-risk populations, including people of color, those with underlying health conditions, and those who are socioeconomically disadvantaged. Ensuring access to COVID-19 vaccines for these communities can help address the disparate health effects of the virus and achieve herd immunity. The Biden administration has identified vaccine equity as a priority, but states and local jurisdictions vary in how and the extent to which they prioritize equity. Given that vaccine roll-out in the U.S. is inherently local, understanding how vaccination rates vary at the local level is important for informing outreach efforts and addressing equity. Earlier CDC analysis found that, as of early March, counties with high social vulnerability had lower vaccination rates than counties with low social vulnerability.
This issue brief builds on that analysis by analyzing how vaccination rates to date vary by counties and identifying key county characteristics that are associated with higher or lower county vaccination rates. It is based on KFF analysis of newly available data from Centers for Disease Control and Prevention (CDC) that shows the percent of the population fully vaccinated at the county-level; the data also provides this share for those ages 65 and older. The CDC data, while incomplete (see methods), provides the first comprehensive data to examine vaccine rollout at the county level. The results in this brief use data as of March 29, 2021 and include 72% of all counties (2,247) in the US. See Methods box for a more detailed discussion of the data, measures included in the analysis, and methodology.
Key Findings
There is wide variation in reported vaccination rates by county across the US. Across the 2,247 counties included in this analysis, the average vaccination rate is 15.8% for the total population and 46.7% for the population 65 and older. Seven of the top ten counties with the highest vaccination rates are in Alaska, where 21.9% of the population is fully vaccinated as of March 28, 2021 (Table 1). Alaska has consistently been at or near the top of states, as ranked by share of population fully vaccinated.
.
.
There are mixed findings on how county vaccination rates align with national prioritization recommendations and state prioritization decisions. The CDC recommended that as long as vaccine supplies were limited, certain groups be prioritized for vaccine access, including healthcare workers and long term care residents, as well as older adults and people with medical conditions that put them at greater risk of severe COVID-19 illness. In addition to healthcare workers and long-term care residents, all states have prioritized vaccinating older adults, and indeed, counties with higher shares of people ages 65 and older have higher vaccination rates (18.2%) than those with lower shares of people ages 65 and older (14.9%). In contrast, most states were slower in opening up eligibility to those with high-risk medical conditions and the list of qualifying conditions differs across states. We found that counties with higher shares of people with certain high-risk medical conditions have a lower average vaccination rate, compared to those with smaller shares (14.0% v 16.7%), suggesting that those who are at greatest risk of severe COVID-19 may be less likely to have been reached thus far.
Additionally, county vaccination rates do not seem directly correlated to COVID-19 impact. Counties with low scores for community transmission of COVID-19, as well as lower COVID-19 deaths per 100,000 people, have higher vaccination rates than counties with high community transmission scores and death rates. The CDC defines community transmission levels for counties based on cases per 100,000 population and shares of positive tests in the past week. Counties classified as having “low” community transmission levels (and thus have lower numbers of cases and positive tests) have an average vaccination rate of 18.3% compared to 15.7% for counties with “high” community transmission levels. Similarly, in the counties with the lowest cumulative deaths per 100,000 people, the average vaccination rate is 16.8% compared to 15.9% in counties with the highest numbers of deaths per 100,000 people.
Providing further evidence of equity concerns in vaccine access, counties with higher shares of Black and Hispanic people, respectively, have lower vaccination rates than counties with lower shares. In counties with high shares of Black people, the vaccination rate is 13.7% compared to 16.4% in in counties with low shares of Black people. There is a smaller difference in vaccination rates among counties with high versus low shares of Hispanic people, with the vaccination rate in counties with higher shares of Hispanic people 15.0% versus 15.9% in counties with low shares of Hispanic people. These findings are consistent with lower vaccination rates among Black and Hispanic people overall. At the same time, while the gap in vaccination rates for Hispanic people disappear in the population 65 and older, it remains for Black people. The average vaccination rate for people 65 and older is the same in counties with high and low shares of Hispanic people (46.7%). However, like vaccination rates for the total population, in counties with high shares of Black people, the vaccination rate for people age 65 and older is lower than in counties with low shares of Black people (44.6% vs. 47.3%).
In addition, higher county uninsured rates and poverty rates are associated with lower vaccination rates. The average vaccination rate in counties with relatively high uninsured rates is 15.3% compared to 17.1% in counties with lower uninsured rates. Higher poverty rates, which are associated with lack of insurance coverage and may contribute to other barriers to accessing vaccines, are also associated with lower county vaccination rates (Appendix Table).
Consistent with CDC’s recent research, counties that rank high on the Social Vulnerability Index (SVI) (those with higher vulnerability) have lower vaccination rates than counties that rank lower on this index (14.1% vs. 17.7%). This finding is not surprising given that SVI aggregates measures of socioeconomic status, age, race/ethnicity, some of which we discuss above, along with additional measures of disability, housing type, and transportation access. Regardless, individuals in counties with higher vulnerability are currently less likely to be vaccinated than those in counties with lower vulnerability.
Metro counties have lower vaccination rates for the total population than non-metro counties and vaccination rates are lower in counties that voted for Trump compared to those that voted for Biden. The share of the total population vaccinated in metro counties is 15.1% compared to 16.3% in non-metro counties. However, the share of the population 65 and older vaccinated is higher in metro counties, 47.5% versus 46.3% in non-metro counties. In addition, consistent with evidence of vaccine hesitancy among Republican voters, the average vaccination rate in counties that voted for Trump is 15.5% compared to 16.3% in counties that voted for Biden.
Conclusion
This analysis of county-level vaccination rates provides further evidence of inequities in COVID-19 vaccination efforts to date. Counties with higher shares of people disproportionately affected by COVID-19, including Black and Hispanic people, people with high-risk medical conditions, and those living in poverty, have lower vaccination rates than counties with lower shares of these populations. These data can be used to help direct continued outreach and vaccination efforts going forward. In addition, we also find that counties with higher levels of community transmission of COVID-19 have lower vaccination rates, suggesting that efforts to accelerate vaccination and stave off rising cases in some areas could be better targeted.
|
This issue brief analyzes data at the county level and draws from multiple sources. – Our main outcome of interest, vaccination rates by county, was collected from the Centers for Disease Control and Prevention’s (CDC) COVID-19 Integrated County View. The CDC data reports completed vaccination rates for total population and population over age 65. Data are not reported for Hawaii, New Mexico, Texas, and California’s smallest counties. In addition, we exclude data for counties where less than 80% of vaccination records include county of residence, which eliminated data for Colorado, Georgia, Nebraska, New Hampshire, South Dakota, Vermont, Virginia, and West Virginia. The analysis includes data for 2,247 counties, 72% of total counties in the US.
– We also use the CDC data for “community transmission level”, which classifies counties based on new cases per 100,000 people and the share of positive tests in the last 7 days. Data to categorize counties by demographic characteristics of residents is pulled from the Census Bureau’s 2019 American Community Survey 5-Year Estimates by county. We use ACS data to categorize counties by residents’ age, race/ethnicity, poverty, and health coverage. Specifically, we calculate the share of the county population that is over age 65, people of color, Non-Hispanic Black, Hispanic, in a family with income below poverty, and is uninsured. Data on the cases and deaths were pulled on March 28, 2021 from the Johns Hopkins University county data. To calculate cases/deaths per 100,000 population, totals for each county were pulled from the Census Bureau’s demographic data – using total population. The 2020 Presidential Election results were pulled from a GitHub repository that compiled data from media sources including The Guardian, townhall.com, Fox News, Politico, and the New York Times. Alaska is excluded from this component of the analysis as the only data available is at the district-level and cannot be cross-walked onto counties. Metro and non-metro classifications are based on the U.S. Department of Agriculture’s 2013 Rural-Urban Continuum Codes. Counties with codes 1 through 3 are classified as “metro” and 4 through 9 are classified as “non-metro.” Data on the share of the population with underlying medical conditions that put them at higher risk for severe COVID-19 illness by county came from the CDC. The conditions included chronic kidney disease, COPD, heart disease, diagnosed diabetes, and obesity (BMI >= 30). County Social Vulnerability Index (SVI) is from the CDC’s Agency for Toxic Substances and Disease Registry. SVI indicates a community’s vulnerability based on certain social conditions (i.e. socioeconomic status, household composition, language, etc.) that may affect the community in the event of a disaster. To classify counties, we translate continuous measures into categorical outcomes, using the group definitions below:
|