Ensuring widespread global access to COVID-19 vaccines, which is necessary for preventing cases and deaths and contributing to global population immunity, is a critical challenge and one that could threaten the ability to control the pandemic. Despite efforts to address vaccine access, most notably through the creation of COVAX, which aims to support the development and delivery of COVID-19 vaccines with a particular focus on assisting low- and middle-income countries, significant disparities remain. The latest data from the Duke Global Health Innovation Center Launch and Scale Speedometer, which monitors COVID-19 vaccine purchases, finds that high-income countries already own more than half of all global doses purchased, and it is estimated that there will not be enough vaccine doses to cover the world’s population until at least 2023.
To further examine the current global distribution of COVID-19 vaccine doses, we used data from the Duke Launch and Scale Speedometer to calculate the share of doses purchased by country income group compared to their share of the global adult population (focusing on adults, ages 18+, because most COVID-19 vaccines are thus far only available for the adult population). In addition, we calculated potential vaccine coverage rates – that is, the share of the adult population that could be fully vaccinated – by country income group. To do so, we reapportioned doses secured through regional agreements to their respective country recipients and added these to individual country totals where bilateral agreements were also in place. While it is not possible to allocate most COVAX doses purchased to individual countries at this time, since COVAX has yet to release its full distribution plan, we did assess how allocating all COVAX doses to low- and middle-income countries (LMICs) would affect these distributions (see Methodology for more detail). Ultimately, we find that without redistribution of doses already purchased by high-income countries (through donations or other means) and/or increased support for manufacturing or production of additional doses, more than four in ten (41%) adults in the world will not be able to be vaccinated, even after allocating all COVAX doses to LMICs.
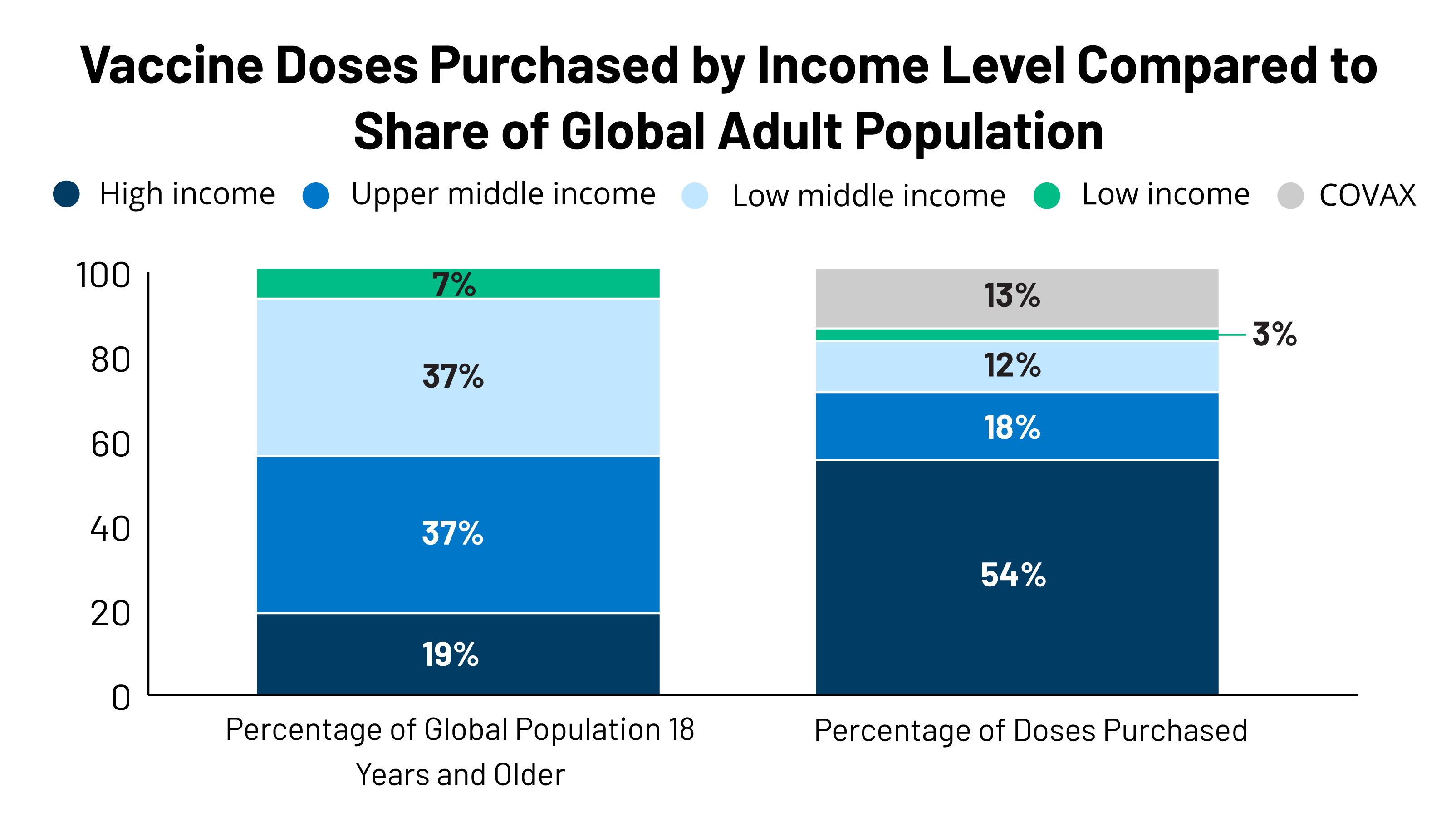
High-income countries, representing just a fifth of the global adult population, have purchased more than half of all vaccine doses, resulting in disparities between adult population share and doses purchased for all other country income groups. We find that although high-income countries only account for 19% of the global adult population, collectively, they have purchased more than half (54%, or 4.6 billion) of global vaccine doses purchased to date. Of the remaining doses, 33% have been purchased by LMICs, who account for 81% of the global adult population; an additional 13% have been purchased by COVAX. Looking by country income group, the largest disparity between doses purchased and population share is for lower-middle-income countries (37% of the global population vs. 12% of purchased doses, or 989 million doses), followed closely by upper-middle-income countries (37% vs. 18%, or 1.5 billion doses). The disparity for low-income countries is smaller (3% vs. 7%, or 263 million doses) (see Figure 1a).
The disparity is even more pronounced when looking at the share who could be vaccinated. While enough vaccine doses have been purchased to cover 80% of the adult population, high-income countries own enough doses to vaccinate more than twice their populations while LMICs can only cover one-third.
High-income countries currently have enough vaccine doses to cover more than twice their adult populations (245% see Figure 2a). Meanwhile, LMICs currently only have enough vaccine doses to reach approximately one-third of their populations, with upper-middle-income countries able to cover 39% of their adult population, low-income countries 38%, and lower-middle-income countries 27%.
Providing all COVAX doses to LMICs could help but would still leave vaccines out of reach for most of the global population. COVAX, which currently accounts for 13% (1.12 billion) of the total number of global doses purchased, has not yet finalized the distribution plan for its full supply, though most doses are expected to be distributed to LMICs. We looked at what would happen to global distribution, relative to population and to vaccine coverage, if all 1.12 billion COVAX doses were provided to LMICs (which is not going to be the case since some will go to high-income countries). While this would result in the share of doses purchased for LMICs increasing from 33% to 46%, it would still be well below their share of the global adult population (81%) (see Figure 1b). Moreover, even with the COVAX doses, less than half (49%) of the adult population in LMICs would be able to be vaccinated (see Figure 2b).
The disparity between vaccines purchased and country income level is significant, but could be addressed in large part through redistribution of doses, as some high-income countries have said they would do. However, such a strategy is highly dependent on the as-of-yet unknown outcomes of several vaccine candidate trials or a significant increase in the manufacturing and production of already authorized vaccines. This analysis demonstrates the significant disparity in vaccine access across much of the world, at least of doses purchased to date. While high-income countries have secured enough doses for more than twice their adult population, LMICs currently have only enough doses to vaccinate just a third, or, if all COVAX doses were allocated to them, still less than a half. Although there are currently enough purchased doses to vaccinate 80% of the global adult population, unless these doses are redistributed, huge inequities in vaccine distribution will persist, presenting a major challenge to achieving global population immunity. Some high-income countries have indicated that they will donate their excess doses, including France, Norway, the U.K., and the U.S. government, which has said it will do so only after it has vaccinated the U.S. population. Still, even if such donations were to occur, their ability to fully address these disparities is in part dependent on the success of some vaccine candidates still in clinical trials or the ability to support the increased manufacturing of or production capacity for already successful vaccine products.
| Methodology |
| We obtained data on COVID-19 vaccine purchases by country from the Duke Global Health Innovation Center Launch and Scale Speedometer. Country income classifications were obtained from the World Bank. Redistributing regional purchases by member country population size was used in order to account for differing income-levels of member countries. Doses secured through regional agreements (made by the African Union, European Union, and Latin America) were reapportioned to their member countries based on adult population size, based on information released about the African Union and European Union. This same method was used for Latin America, although information on how vaccines would be distributed has not been made available. For the Latin America agreement, we included all countries classified as “Latin America and the Caribbean” by the United Nations Department of Economic and Social Affairs, excluding Brazil as specified in the agreement. Territory population totals were not included in our calculations. Population data were obtained from the United Nations Department of Economic and Social Affairs. Since vaccines are currently only being authorized or approved for and provided to adults, with the exception of the Pfizer vaccine which has been approved for individuals 16 years and older, we used population estimates for those 18 years and older. Finally, to estimate potential vaccine coverage by country, we took into account the number of doses needed for full vaccination, depending on the product. For the COVAX reapportionment scenarios, we assumed that all doses currently purchased by COVAX will be allocated to LMICs, even though some of these doses will be distributed to high-income countries, to provide a hypothetical “best-case scenario” for LMICs. |